This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
HALL TICKET NUMBER: 1701006078
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
CASE DISCUSSION:
A 50 years old gentleman, farmer by occupation, resident of Yadadri Bhuvanagiri district came to the hospital with the following cheif complaints.
CHEIF COMPLAINTS:
- Distension of abdomen since 7 days
- Pain in the abdomen since 4 days and
- Pedal edema since 3 days
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 6 months back then he developed jaundice and he was treated for jaundice by a private medical practitioner. After that he was normal till last week.
He developed distension of abdomen 7 days back, which is insidious in onset, gradually progressive, aggravated in last 4 days and progressed to the present size. No aggravating and releiving factors.
He complaints of abdominal pain from last 3 days which is insidious in onset, gradually progressive, in the epigastrium and right hypochondrial regions without any aggravating and releiving factors.
He also complains of swelling in both feet of Grade II since 3 days which is insidious in onset, gradually progressive, pitting type without any aggravating and releiving factors.
NO history of hemetemesis, melena, vomitings, nausea
NO history of bulky stools, black tarry and clay colored stools
NO history of fever with chills and rigor
NO history of anorexia, facial puffiness, generalised edema
NO history of evening rise of temperature, cough, night sweats
NO history of orthopnea, palpitations
NO history of loss of weight
PAST HISTORY:
NO history of similar complaints in the past.
Not a known case of Diabetes, Hypertension, Tuberculosis, Asthma, epilepsy, hypothyroidism/hyperthyroidism, COPD, CAD and blood transfusions.
FAMILY HISTORY:
None of the patient's parents, siblings or first degree relatives have or had similar complaints or any significant comorbidities.
PERSONAL HISTORY:
Appetite: reduced
Diet: mixed
Bladder habits: frequency of urine is reduced since 2 days
Bowel habits: constipation since last 4 days
Sleep: Adequate
Addictions:
- Beedi smoker: for past 30 years. 4-5 beedis per day
- Alcoholic: chronic alcoholic previously
From last one year, occasional alcoholic - consumes 90ml of whiskey
GENERAL PHYSICAL EXAMINATION:
Patient is conscious, coherent and cooperative.
Examined after taking vaild informed consent in a well enlightened room.
Built and nourishment: moderately built and moderately nourished
Pallor: No pallor
Icterus: No icterus
Cyanosis: No cyanosis
Clubbing: No clubbing
Generalised lymphadenopathy: No generalised lymphadenopathy
Pedal edema: Grade II bilateral pedal edema
VITALS:
Temperature: afebrile
Pulse rate: 90bpm, regular rhythm, normal volume
Respiratory Rate: 22 breathes per minute, abdominothoracic type
Blood Pressure: 130/90 mm of Hg in right arm in sitting position
GRBS: 90mg/dl
SpO2: 98% at room air
TREMORS: present
SYSTEMIC EXAMINATION:
PER ABDOMINAL EXAMINATION:
INSPECTION: 9 regions
Shape of the abdomen: globular
Distension of abdomen: distended
Flanks: full
Umbilicus:
Shape: everted
Position: central
Herniations: absent
Discharge: absent
Skin over abdomen: smooth and shiny
No pigmentations, discolorations, scars, sinuses, fistulae, engorged veins, visible pulsations, hernial orifices,
Genitals: normal
PALPATION:
No local rise of temperature
Tenderness: present in the epigastrium region
Hepatomegaly: absent
Splenomegaly: absent
Guarding: present
Rigidity: absent
Renal angle tenderness: absent
No rebound tenderness
No visible peristalsis
FLUID THRILL(with extended legs): POSITIVE
PERCUSSION:
In supine position,
Tympanic note - heard at midline of the abdomen
Dull note - heard at flanks
Shifting dullness: POSITIVE
Liver span : could not be detected
AUSCULTATION:
Bowel sounds: decreased
No bruits
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm medial to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
RESPIRATORY SYSTEM:
Inspection:
Shape- elliptical
B/L symmetrical ,
Both sides moving equally with respiration .
Palpation:
Trachea - central
Expansion of chest is symmetrical.
Vocal fremitus - normal
Percussion: resonant bilaterally
Auscultation:
bilateral air entry present. Normal vesicular breath sounds heard.
CENTRAL NERVOUS SYSTEM
Higher mental functions :-
Patient is conscious ,coherent and cooperative
Right handed individual
Memory - immediate , short term and long term memory are assessed and are normal
Language and speech are normal
Cranial nerves :- intact
Sensory system :-
Sensation right left
Touch felt felt
Pressure felt felt
Pain
-superficial felt felt
-deep felt felt
Proprioception
-joint position ✔ ✔
-joint movement ✔ ✔
Temperature felt felt
Vibration felt felt
Stereognosis ✔ ✔
Motor system
Right. Left
BULK
Upper limbs. N N
Lower limbs N N
TONE
Upper limbs. N N
Lower limbs. N N
POWER
Upper limbs. 5/5 5/5
Lower limbs 5/5 5/5
Gait :- Normal
Superficial and deep reflexes are elicited
No signs ssuggestive of cerebellar dysfunction
INVESTIGATIONS:
1. HEMOGRAM:
Hemoglobin : 9.8 g/dl
TLC : 7,200
Neutrophils : 49%
Lymphocytes : 40%
Eosinophils : 1%
Basophils : 0%
PCV : 27.4%
MCV : 92.3 fl
MCH : 33 pg
MCHC : 35.8%
RDW-CV : 17.6%
RDW-SD : 57.8 fl
RBC count : 2.97 millions/mm3
Platelet count : 1.5 lakhs/mm3
Smear : Normocytic normochromic anemia
2. Serology :
HbsAg : Negative
HIV : Negative
3. ESR :
15mm/1st hour
4. Prothrombin time : 16 sec
5. APTT : 32 sec
6. Serum electrolytes :
Sodium : 133 mEq/L
Potassium : 3 mEq/L
Chloride : 94 mEq/L
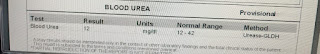
7. Blood Urea : 12 mg/dl
8. Serum Creatinine : 0.8 mg/dl
9. LFT :
Total Bilirubin : 2.22 mg/dl
Direct Bilirubin : 1.13 mg/dl
AST : 147 IU/L
ALT : 48 IU/L
ALP : 204 IU/L
Total proteins : 6.3 g/dl
Serum albumin : 3 g/dl
A/G ratio : 0.9
10. Ascitic fluid :
Protein : 0.6 g/dl
Albumin : 0.34 g/dl
Sugar : 95 mg/dl
LDH : 29.3 IU/L
SAAG : 2.66 g/dl
ASCITIC FLUID CYTOLOGY:
Microscopy:
Cytology smear study shows few scattered lymphocytes, reactive mesothelial cells against a granular eosinophilic proteinaceous background.
No atypical cells are seen.
Impression: negative for malignancy
ASCITIC FLUID CULTURE AND SENSITIVITY REPORT:
ZN staining: No acid fast bacilli seen.
Few epithelial cells with no inflammatory cells seen. No organisms seen.
No growth after 48 hours of aerobic incubation
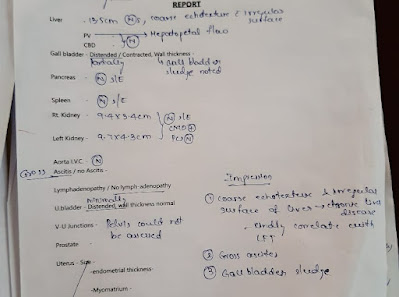
ULTRASONOGRAPHY:
Coarse echotexture and irregular surface of liver - Chronic liver disease
Gross ascites
Gallbladder sludge
ELECTROCARDIOGRAPHY:
CHEST RADIOGRAPHY:
ASCITIC FLUID TAPPING: Done twice
Severity of liver disease:
CHILD-PUGH-TURCOTTE SCORING SYSTEM:
Parameter points asigned
1 2 3
Ascites absent slight moderate
Bilirubin(mg/dl) <2 2-3 >3
Albumin(g/dl) >3.5 2.8-3.5 <2.8
Prothrombin time <4 4-6 >6
Encephalopathy None Grade 1-2 grade 3-4
Interpretation:
Total score: 5-6 well compensated disease
7-9 significant functional compromise
10-15 decompensated disease
In this patient,
Ascites - moderate(3)
Bilirubin- 2.22mg/dl (2)
Albumin - 3g/dl (2)
Prothrombin time- 16 seconds (3)
Encephalopathy- none(1)
Total score: 11
Therfore this patient's liver condition is in Decompensated state.
PROVISIONAL DIAGNOSIS:
This is a case of Decompensated Chronic liver disease with ascites, probably secondary to chronic alcoholism.
TREATMENT:
1. Inj. PANTOPRAZOLE 40 mg IV OD
2. Inj. LASIX 40 my IV BD
3. Inj. THIAMINE 1 Amp in 100 ml IV TID
4. Tab. SPIRONOLACTONE 50 mg BB
5. Syrup. LACTULOSE 15 ml HS
6. Syrup. POTCHLOR 10ml PO TID
7. Fluid restriction less than 1L/day
8. Salt restriction less than 2g/day

























Comments
Post a Comment