GENERAL MEDICINE PREFINAL CASE
28 YEARS OLD MALE WITH ACUTE PANCREATITIS SECONDARY CHOLELITHIASIS
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs".
This E log book also reflects my patient-centered online learning portfolio and your valuable comments on comment box is welcome.
Name: KASTURI VIJAY KUMAR
Roll no: 56
MEDICINE CASE DISCUSSION:
A 28 years old tailor hailing from Urban Telangana has presented with complaints of pain abdomen since 2 days
HISTORY OF PRESENTING ILLNESS:
The patient was apparently in his normal state of health 8 years ago.Then he developed pain abdomen which was sudden in onset colicky type, aggravated on taking fatty food and relieved on medication, for which he went to a local hospital where he was evaluated and he was diagnosed with Gall stones. Then he was referred to a higher centre where MRCP was done as a therapeutic procedure. After which he was apparently normal for some months following which he developed similar episodes of pain frequently (twice in 5 months) for which consulted a local RMP for which he was given some medications (unknown).
About 2 days ago he was having a similar episode of pain abdomen which was continuous, colicky type, shooting to the back in standing position. It was relieved temporarily after bending forwards for some time. He says that he feels more comfortable when he raises his legs or bends forward He also gives history of 2 episodes of vomiting which was projectile, and has food as content.
No history of loss of appetite but he avoids taking food as pain aggravates on consumption of food.
No history of jaundice, bowel disturbances, burning micturition and trauma
PAST HISTORY:
MRCP and ERCP done for Gall stones 8 years ago.
No history of Diabetes ,hypertension ,asthma, TB, epilepsy , CAD
PERSONAL HISTORY :
Appetite :- Good but avoids eating because of pain
Diet :- Mixed
Bowel and bladder :- Regular
Sleep :- Adequate
Addictions:- nil
FAMILY HISTORY:
No history of similar complaints
GENERAL PHYSICAL EXAMINATION :
Patient was examined in a well lit room after obtaining valid informed consent and Adequate exposure
He is conscious, coherent, cooperative
Well oriented to time place person
Moderately built and nourished
Pallor :- no pallor
Icterus:- no icterus
Cyanosis:- no cyanosis
Clubbing :- no clubbing
Generalised Lymphadenopathy:-no generalised Lymphadenopathy
Pedal edema:- no pedal edema
VITALS :
Temperature :- afebrile
Respiratory rate :-14 cycles per minute
Pulse:- 86 beats per minute, regular,normal in volume and character, no vessel wall thickening, no radioradial delay
Blood pressure :- 130/80 mmHg sitting position in right arm
SYSTEMIC EXAMINATION :
PER ABDOMEN:
Inspection:
The abdomen is scaphoid
Umbilicus is central
Mild distension in Epigastric area and flanks are normal
Skin is normal and shiny
Abdomen wall movements normal with respiration
No engorged veins
No divarication of recti
No visible pulsations
No visible peristalsis
No scars and sinuses
Herinal orifices are free
Cullens sign :-absent
Gray turner sign:- absent
Fox sign :- absent
Bryant sign :- absent
Palpation:
No local rise of temperature
Tenderness on epigastrium
All Inspectory findings are confirmed
On deep Palpation, Liver, gall bladder and spleen are not palpable
No guarding , rigidity , palpable masses
Murphys sign :- absent
Measurements:-
Abdominal girth at level of umbilicus :- 33 inches
Percussion :-
Tympanic note heard all over abdomen
Shifting dullness absent
Fluid thrill absent
Auscultation:-
Bowel sounds appreciated
No abnormal sounds heard
RESPIRATORY SYSTEM:
Inspection
Chest is bilaterally symmetrical
The trachea appears to be in centre
Apical impulse is not appreciated
Chest moves equally with respiration on both sides
No dilated veins, scars or sinuses are seen
Palpation-
Trachea is felt
Chest moves equally on both sides on respiration
Apical impulse is felt in the fifth intercostal space 1cm lateral to mid clavicular line
Tactile vocal fremitus- appreciated
Percussion-
The areas percussed include the supraclavicular, infraclavicular, mammary, axillary, infraaxillary, suprascapular, infrascapular areas.
They are all resonant.
Auscultation-
Normal vesicular breath sounds are heard
No adventitious sounds
CARDIOVASCULAR SYSTEM-
Inspection-
The chest wall is bilaterally symmetrical
No dilated veins, scars or sinuses are seen
Apical impulse or pulsations cannot be appreciated
Palpation-
Apical impulse is felt in the fifth intercostal space, 1 cm lateral to the midclavicular line
No parasternal heave felt
No thrill felt
Percussion-
Right and left borders of the heart are percussed
Auscultation-
S1 and S2 heard, no added thrills and murmurs are heard
CENTRAL NERVOUS SYSTEM-
HIGHER MENTAL FUNCTIONS:
Patient is Conscious, well oriented to time, place and person.
All cranial nerves - Intact
No signs of meningeal irritation
Motor system
Right. Left
BULK
Upper limbs. N. N
Lower limbs N. N
TONE
Upper limbs. N. N
Lower limbs. N. N
POWER
Upper limbs. 5/5. 5/5
Lower limbs 5/5. 5/5
Superficial reflexes and deep reflexes are present, normal
Gait- normal
No involuntary movements
Sensory system- All sensations (pain, touch, temperature, position, vibration sense) are well appreciated
INVESTIGATIONS:
Pancreatic enzymes
S. Amylase 124 IU/L(normal-13-60)
S. Lipase 528IU/L(normal-25-140)
HEMOGRAM-
HB 16.3grm/dl
TC 17,100cells/cumm (normal-4000-10000)
PLT 3.38
MCV 82.5
PCV 46
MCH 29.2
MCHC 35.4
SMEAR - NORMOCYTIC NORMOCHROMIC
BGT- O positive
RBS- 124
RFT-
Urea 50mg/dl (normal-12-42)
Creatinine 0.9mg/dl (normal-0.9-1.3)
S. Sodium 140mEq/L(normal-136-145)
S. Potassium 3.8mEq/L(normal-3.5-5.1)
S. Chloride 98mEq/L(normal-98-107)
LFT-
TB 1.38mg/dl (normal 0-1)
DB 0.45 mg/dl(normal-0.0-0.2)
AST 36 IU/L(normal-0-31)
ALT 21IU/L (normal-0-34)
ALP 117IU/L(normal-42-98)
TP 6.7gm/dl(normal-6.4-8.3)
ALB 3.73gm/dl(normal-3.5-5.2)
SEROLOGY: NEGATIVE
BLOOD SUGAR LEVELS:
RBS-124mg/dl
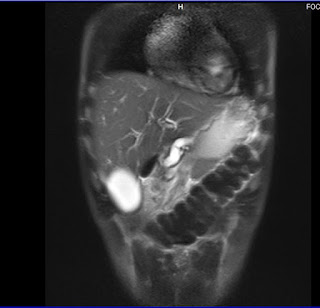
USG Abdomen
CHEST X RAY:
Provisional diagnosis
Acute pancreatitis secondary to chronic cholelithiasis
TREATMENT:
Diet :-
On 30/3/2022 he was kept on Nill per mouth
On 31/3/2022 he was given soft food
Medical management
1. Inj . Tramadol
2. IV fluids :- RL and NS 100 ml / hr






















Comments
Post a Comment