75 YEARS OLD MALE WITH COMMUNITY ACQUIRED PNEUMONIA WITH CHRONIC KIDNEY DISEASE
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs".
This E log book also reflects my patient-centered online learning portfolio and your valuable comments on comment box is welcome.
MEDICINE CASE DISCUSSION:
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
VIEW OF THE CASE :
A 75 years old male came with the cheif complaints of shortness of breathe since 5 hours, loose stools of 3 episodes from today and fever since 6 days.
HISTORY OF PRESENT ILLNESS:
Patient was a mason by occupation and stopped doing work since 10 years. He was normal with his daily routine 6 days back, then he developed fever of low grade , intermittent, releived on taking medication and not associated with any chills and rigors.
He had constipation for 2 days and received DULCOLEX tablets and developed loose stools of 3 episodes.
From 5 hours, he is having shortness of breathe of grade 3 and often irritable.
PAST HISTORY:
He is a known case of Hypertension since 1 year. And receiving TAB. AMLODIPINE 5mg .
He is diagnosed for TUBERCULOSIS 30 years back and took treatment for 2 years.
He is not a known case of diabetes, asthma, epilepsy
1 year back, because of repeated falls, went to government hospital initially diagnosed as hypotensive and after 5 months he was diagnosed as hypertensive and started medications for that.
1 year back, he had pedal edema and shortness of breathe, diagnosed as renal failure and received conservative treatment fo 4 months and stooped medications. Only TAB. NODOSIS is continued till now.
PERSONAL HISTORY:
Appetite- decreased appetite since suffering from fever
Diet- mixed
Bowel habits- loose stools of 3 episodes
Bladder habits- regular
Sleep- disturbed due to dyspnea
Addictions-
Smoking- 18 beedi/day smoked for 30 years and stopped smoking after diagnosed as tuberculosis.
Alcohol- takes 90ml/day and stopped taking regularly 1 year back and taking occasionally on social gatherings.
Allergies- no allergies
FAMILY HISTORY:
Insignificant
GENERAL EXAMINATION:
Conscious and irritable
Pallor- no pallor
Icterus- no icterus
Cyanosis- no cyanosis
Clubbing- no clubbing
Generalised lymphadenopathy-no generalised lymphadenopathy
Pedal edema- no pedal edema
VITALS:
Temperature- 98.4°F
Pulse rate- 92bpm
Respiratory Rate- 22/min
Blood Pressure- 150/70 mm Hg
SpO2- 90%
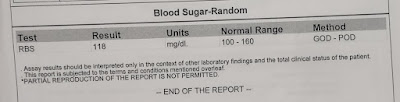
GRBS- 120mg%
SYSTEMIC EXAMINATION:
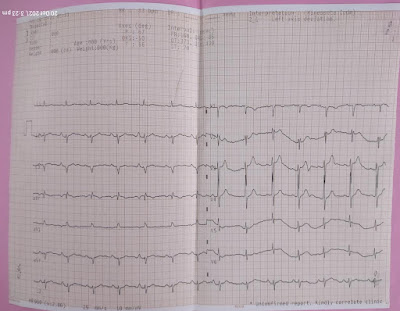
CARDIOVASCULAR SYSTEM:
First and second heart sounds heard and no murmurs.
RESPIRATORY SYSTEM:
Dyspnea- present of 3rd grade
Wheeze - present
Vesicular breath sounds
Rhonchi heard at right infra axillary area
CENTRAL NERVOUS SYSTEM:
Conscious
Speech- normal
No neck stiffness and kernings sign is negative
Cranial nerves, motor and sensory systems are normal
PER ABDOMEN EXAMINATION:
shape - scaphoid
No tenderness
No palpable mass
No hernial orifices
No bruits
No palpable liver and spleen
INVESTIGATIONS:
HEMOGRAM
COMPLETE URINE EXAMINATION
RANDOM BLOOD SUGAR
SERUM UREA
SERUM CREATININE
SERUM ELECTROLYTES
LIVER FUNCTION TEST
ARTERIAL BLOOD GAS
ELECTROCARDIOGRAPHY
CHEST X RAY
ULTRASONOGRAPHY:
SEROLOGY:
DIAGNOSIS:
COMMUNITY ACQUIRED PNEUMONIA OF LEFT LOBE WITH CKD WITH HYPERTENSION
TREATMENT:
- INJ. AUGMENTIN 1.2mg/IV/BD
- TAB. AZITHROMYCIN 500mg /PO/BD
- HEAD END ELEVATION
- OXYGEN SUPPLEMENTATION IF SPO2 <90%
- FLUID RESTRICTION <1 LITRE/DAY
- SALT RESTRICTION <2.4GRAM/DAY
- TAB. AMLODIPINE 5mg/PO/OD
- TAB. NODOSIS 500mg /PO/OD
- NEB WITH DUOLIN 6TH HOURLY, BUDECORT 6TH HOURLY
- INTERMITTENT CPAP 2ND HOURLY
- TAB. DOLO 650mg /PO/SOS
- MONITOR VITALS 4TH HOURLY
- TEMPERATURE CHARTING 4TH HOURLY
- STRICT INPUT/OUTPUT CHARTING

























Comments
Post a Comment