75 YEARS OLD MALE WITH COUGH, FEVER AND SOB
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Presenting complaints:
A 75 years old gentleman came with the cheif complaints of cough, fever and shortness of breath since 2 days.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic 2 days back then he developed cough which is dry type
Complaints of fever which is of high grade, gradually progressive associated with chills and rigors, releived by taking medication.
Complaints of shortness of breath since 2 days which is GRADE II gradually progressed to GRADE III. No orthopnea, no PND. No pedal edema
No JVP, no chest pain, no palpitations, no tremors, no burning micturition. Increased output of urine since 2 days.
PAST HISTORY:
No h/o similar complaints in the past 1 year back.
Not a known case of diabetes, hypertension, tuberculosis, epilepsy, bronchial asthma, CAD, CVD
PERSONAL HISTORY:
Shepherd by occupation.
loss of appetite since 3 months
Increased frequency of micturition
No addictions.
GENERAL PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy
VITALS:
TEMPERATURE: 98°F
PULSE RATE: 91bpm
RESPIRATORY RATE: 25cpm
BLOOD PRESSURE: 170/100mm Hg
SPO2: 96% @ room air
GRBS: 98mg/dl
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
RESPIRATORY SYSTEM:
CENTRAL NERVOUS SYSTEM:
PER ABDOMEN:
General surgery referral have been taken in view of bloating and tightness of abdomen and advised for x ray abdomen erect and further observation.
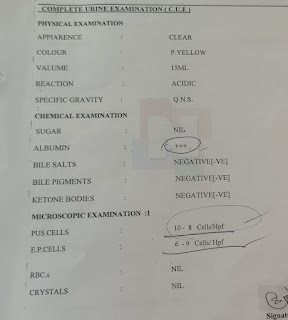
INVESTIGATIONS:
CHEST X RAY:
ELECTROCARDIOGRAPHY:
ULTRASOUND:
NO SONOLOGICAL ABNORMALITY DETECTED
ARTERIAL BLOOD GAS ANALYSIS
PROVISIONAL DIAGNOSIS:
ACUTE EXACERBATION OF COPD
TREATMENT:
1. OXYGEN INHALATION TO MAINTAIN SPO2 MORE THAN 94%
2. INJ. PAN 40 MG IV/OD
3. INJ. ZOFER 4MG IV/SOS
4. INJ. OPTINEURON 1 AMP IN 500ML NS IV/OD
5. INJ. NEOMOL IGM IV/SOS IF TEMPERATURE MORE THAN 101°F
6. NEBULIZATION WITH BUDECORT 6TH HOURLY AND DUOLIN 8TH HOURLY
7. INJ. HYDROCORTISONE 100MG IV/SOS
8. VITALS MONITORING AND INFORM SOS












Comments
Post a Comment