60 YEARS OLD MALE WITH EDEMA OF BOTH UPPER AND LOWER LIMBS
This is an online E-log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent. Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs.
This E log book also reflects my patient centered online learning portfolio and your valuable comments on comment box is welcome.
I have been given this case to solve in an attempt to understand the topic of " patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with diagnosis and treatment plan.
Presenting complaints:
A 60 year old gentleman came to the casualty with the cheif complaints of edema of both upper and lower limbs since 10 days,complaints of facial swelling decreased urine output since yesterday, vomiting of 6 episodes since yesterday, loose stools of 4 episodes since today morning.
HISTORY OF PRESENT ILLNESS:
Patient was apparently alright 2 years back then he had altered sensorium and was diagnosed to have ?DKA, given insulin and treated
After that 10 days patient developed swelling of lower limbs and ulceration on right toe and plantar aspect of foot for which he was treated.
3 months back patient developed nausea, vomiting 2 episodes/day. Food particles as content, non projectile followed by altered sensorium secondary to hyponatremia?SIADH with HYPOKALEMIA. Patient admitted in the hospital on 23rd December and got discharged on 31st December 2023.
4 years back patient developed giddiness and while walking patient had fall and fracture of right upper and right lower limb.
Presently patient complaints of bilateral pedal edema since 10 days for which he admitted in government hospital. Condition worsened and swelling of face bilateral upper limb started 4 days back .
Complaints of decreased urine output since yesterday
Associated with 6 episodes of vomiting food particles as content non bilious non projectile
4 episodes of loose stools watery non blood stained
No history of fever, palpitations, sob, pain abdomen, sweating, burning micturition
PAST HISTORY:
History of similar complaints in the past and admitted in the hospital on 23rd December 2022 and discharged on 31 December 2022. There was history of altered sensorium present at the time of previous hospitalisation.
Known case of diabetes from 10 years. On Tab. Glimipride 1mg before breakfast and Tab. Metformin 500 mg after breakfast.
Known case of hypertension since 4 years. On Tab. Telma H(TELMISARTAN 40 mg+ hydrochlorthiazide 12.5mg) in morning and Tab. Cilacar 10mg at night.
Not a known case of tuberculosis, bronchial asthma, CAD, CVD
PERSONAL HISTORY:
Farmer by occupation. Stopped since 4 years
Appetite decreased from 4 days
Decreased urine output since yesterday
Known alcoholic. Stopped from 10 years
Known smoker stopped since 10 years
GENERAL PHYSICAL EXAMINATION:
Patient is conscious coherent and cooperative
No signs of pallor, icterus, cyanosis, clubbing, generalised lymphadenopathy
VITALS:
TEMPERATURE: 97.4°F
PULSE RATE: 90bpm
RESPIRATORY RATE: 18cpm
BLOOD PRESSURE: 140/80mm Hg
SPO2: 97% @ Room air
GRBS:306mg/dl
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
First and second heart heart sounds heard.
Jvp not raised
RESPIRATORY SYSTEM: Bilateral air entry present. Clear
CENTRAL NERVOUS SYSTEM: higher mental functions normal.
PER ABDOMEN: soft non tender.
INVESTIGATIONS:
CHEST X RAY:
ELECTROCARDIOGRAPHY:
2D ECHOCARDIOGRAPHY:
2DECHOCARDIOGRAPHY:
https://youtube.com/shorts/4ZWev_AkXOE?feature=share
TRIVIAL TR+/AR+: NO MR
NO RWMA. NO AS/MS. SCLEROTIC AV
GOOD LV SYSTOLIC FUNCTION
DIASTOLIC DYSFUNCTION. NO PAH
ULTRASOUND:
IMPRESSION:
BILATERAL RENAL CORTICAL CYSTS
BILATERAL RAISED ECHOGENECITY OF KIDNEYS
INCREASED URINARY BLADDER WALL THICKNESS
CORRELATE WITH CUE TO RULE OUT CYSTITIS
SEROLOGY:
HCV:NON REACTIVE
HIV: non reactive
HBSAG: negative
SERUM OSMOLARITY
BUN/CREATININE: 12.6
FBS: 161mg/dl
PLBS: 219mg/dl
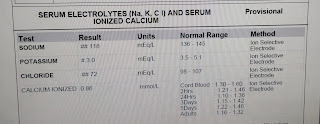
Serum electrolytes on 13/03/2023
URINARY ELECTROLYTES:
ABG:
Serum electrolytes:
RFT:
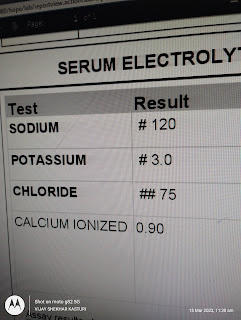
On 14/03/2023
S. Urea:42mg/dl
S. Creatinine: 1.5mg/dl
S. Na+:119mEq/L
S. K+: 2.7mEq/L
S. Cl-: 78mEq/L
S. Ca+2: 0.90 mmol/L
On 14/03/2023
S. Na+:118mEq/L
S. K+: 3.2mEq/L
S. Cl-: 76mEq/L
S. Ca+2: 0.80 mmol/L
On 1503/2023
S. Urea:45 mg/dl
S. Creatinine: 1.4mg/dl
S. Na+:116mEq/L
S. K+: 3.2mEq/L
S. Cl-: 80 mEq/L
S. Ca+2: 0.91 mmol/L
PROVISIONAL DIAGNOSIS:
HYPOOSMOLAR HYPERVOLEMIC HYPONATREMIA WITH HYPOKALEMIA WITH ACUTE KIDNEY INJURY(RENAL) WITH K/C/O DIABETES AND HYPERTENSION WITH MILD ANEMIA
TREATMENT:
1. FLUID RESTRICTION
2. INJ. KCL 20mEq IN 100ML NS @ 20ml/hr
3. TAB. GLICLAZIDE 40 MG PO/OD
4. TAB. TELMA 40 MG PO/BD
5. TAB. MET XL 25 MG PO/BD
6. VITALS MONITORING
7. 7 POINT GRBS MONITORING.
8.TAB. CILINDIPINE 10MG PO/BD
9. INPUT OUTPUT CHARTING
10. SYRUP. POTCHLOR 15ML PO/TIDVIN 1 GLASS OF WATER
11. INJ. ZOFER 4 MG IV/SOS
12. INJ. PAN 40 MG IV/OD
13. TAB. ALDACTONE 50 MG PO/OD




































Comments
Post a Comment