GENERAL MEDICINE PREFINAL CASE
36 YEAR OLD MALE WITH ACUTE PANCREATITIS WITH ALCOHOL DEPENDENCE SYNDROME
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs".
This E log book also reflects my patient-centered online learning portfolio and your valuable comments on comment box is welcome.
Name: KASTURI VIJAY KUMAR
Roll no: 56
MEDICINE CASE DISCUSSION:
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
VIEW OF THE CASE:
A 36 years old gentleman resident of manchala mandal of Rangareddy district, police jeep driver by occupation came to the hospital on 3rd January with the chief complaints of pain abdomen from 1st January, belching from 1st January.
HISTORY OF PRESENT ILLNESS:
Patient was apparently asymptomatic till 28th December, then from 29th December he started taking alcohol in excess amount till 31st December. From 1st January, he started experiencing pain in the abdomen which is dragging type, sudden in onset rapidly progressive, without any aggravating and releiving factors and not radiating.
Associated with profused sweating
Patient also complaints of increased belching from 1st January.
No history of nausea, vomitings, fever, chills
No history of decreased appetite, previous jaundice episodes,pruritis
No history of constipation, fatty stools, malena
No history of oliguria, hematuria, involuntary movements, tremors, altered sleep
PAST HISTORY:
Similar episode of pain abdomen in last June. And releived the next day.
He was traumatised twice in the past after consuming alcohol.
First incident: 10 years back - got injuries to nose, mouth and tongue and sutured for tongue injuries.
Second incident- in June 2020, after some occupational issues.
Past medical history: not a known case of diabetes, hypertension, tuberculosis, asthma, thyroid disorder, seizures,
Past surgical history: no significant surgical history.
FAMILY HISTORY: Insignificant
PERSONAL HISTORY:
Appetite: decreased appetite after alcohol intake and normal in abstinence
Diet : mixed
Bladder habits: regular
Bowel habits: regular
Sleep : Adequate
Addictions:
Chronic alcoholic since 10 years
Consumes whisky
Atleast 5 times/week
Consumes 180ml minimum per sitting
No other addictions
GENERAL PHYSICAL EXAMINATION:
Conscious, coherent and cooperative
Moderately built and moderately nourished
Consent-taken
Examined in a well lit room
Pallor- no pallor
Icterus- present
Cyanosis- no cyanosis
Clubbing- no clubbing
Koilonychia- no koilonychia
Generalised lymphadenopathy- no generalised lymphadenopathy
Pedal edema- no pedal edema
VITALS:
Temperature: afebrile
Pulse rate: 86bpm, regular, normal volume measured in radial artery in sitting position
Respiratory rate: 16 cycles per minute
Blood Pressure: 140/110 mm of Hg measured in left arm in sitting position.
SpO2: 98% at room air
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM: First and second heart sounds heard. No murmurs
RESPIRATORY SYSTEM: Normal vesicular breath sounds with bilateral air entry present
CENTRAL NERVOUS SYSTEM: no focal neurological deficit and normal higher mental functions with
PER ABDOMEN EXAMINATION:
INSPECTION: All 9 regions
Shape: globular (protuberant)
Distension: distended
Flanks: full
Guarding: present
Umbilicus- central, inverted
Skin: normal, shiny with scar of previous injury, no pigmentation, no engorged veins
Divarication of recti: absent
Dilated veins: absent
Abdominal wall movements: normal with respiration
No visible gastric peristalsis
No hernial orifices and cough impulse
External genitalia: normal
Cullen sign: absent
Gray turner sign: absent
Fox sign: absent
Bryant sign: absent
PALPATION:
No Local rise of temperature
Tenderness: tender abdomen in epigastrium, right hypochondrium, right lumbar and umbilical regions
No guarding, rigidity and palpable masses
Liver: no hepatomegaly
Spleen: no splenomegaly
Gall bladder: not palpable
Murphy sign: absent
Measurements:
Abdominal girth at the umbilicus: 38 inches
Xiphisternum to umbilicus: 9 inches
Umbilicus to pubic symphysis: 5 inches
Spinoumbilical : 19 inches
PERCUSSION:
Shifting dullness: absent
Fluid thrill : absent
Liver span: normal
Spleen span: normal
AUSCULTATION:
bowel sounds: normal
No abnormal sounds heard
INVESTIGATIONS:
SERUM AMYLASE:223
SERUM LIPASE:86.1
LIVER FUNCTION TEST:
ULTRASONOGRAPHY ABDOMEN
CHEST X RAY:
COMPLETE BLOOD PICTURE
COMPLETE URINE EXAMINATION
RENAL FUNCTION TEST
HEMOGRAM
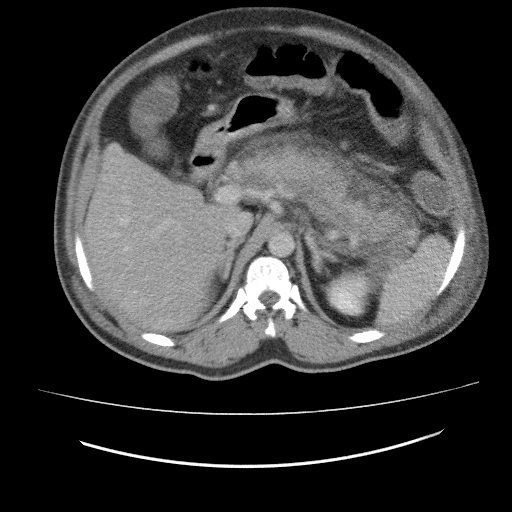
CT (PLAIN AND IV CONTRAST): ABDOMEN AND PELVIS
ELECTROCARDIOGRAPHY
2D ECHOCARDIOGRAPHY :
BISAP SCORE:
B- Blood urea nitrogen>25mg/dl -0
Impaired mental status- 0
Systemic inflammatoryresponsesyndrome-0
Age>60 years -0
Pleural effusion-1
Total BISAP score = 1
PSYCHIATRIC REFERRAL:
DIAGNOSIS:
ACUTE PANCREATITIS WITH ALCHOL DEPENDENCE SYNDROME
TREATMENT:
1. IV FLUIDS NS/RL/DNS AT 50ml/hour
2. INJ. PANTOP 40 mg IV/OD
3. INJ. ZOFER 4mg IV/SOS
4. INJ. TRAMADOL 1 AMPOULE IN 100ml NS OD
5. INJ. BUSCOPAN 2CC IV/SOS
6. TAB. PARACETAMOL 500mg PO/SOS
7. THIAMINE
8. RYLES TUBE
9. SOAP WATER ENEMA
10. INPUT AND OUTPUT CHARTING
11. TEMPERATURE CHARTING
12. GRBS 6TH HOURLY




















Comments
Post a Comment