40 YEARS OLD MALE WITH ANASARCA SECONDARY TO RIGHT HEART FAILURE WITH WET BERIBERI
This is an online E log book to discuss our patient's de-identified health data shared after taking his/her/guardian's signed informed consent.Here we discuss our individual patient's problems through series of inputs from available global online community of experts with an aim to solve those patient's clinical problems with collective current best evidence based inputs".
This E log book also reflects my patient-centered online learning portfolio and your valuable comments on comment box is welcome.
MEDICINE CASE DISCUSSION:
I've been given this case to solve in an attempt to understand the topic of "Patient clinical data analysis" to develop my competency in reading and comprehending clinical data including history, clinical findings, investigations and come up with a diagnosis and treatment plan.
VIEW OF THE CASE:
A 40 yr old male, Auto driver by occupation, resident of chityala, came to casualty with
Cheif Complaints of
- Generalised swelling & swelling of hands & legs since 1 week
HISTORY OF PRESENT ILLNESS:
Patient came to the casuality with pedal edema since 1week,which was Insidious in onset, gradually progressed to upper abdomen & developed anasarca associated with Shortness of breathe(SOB) (GRADE-IV),
Orthopnoea(discomfortwhen breathingwhile lying down) - present
Dry cough - Present
PND(paroxysmal nocturnaldyspnoea) - Absent
- H/O daily intake of alcohol since 13 yrs (daily 90- 180ml) present
PAST HISTORY:
Patient was apparently asymptomatic 2 years back, then he had pedal edema which is bilateral Pitting type, Insidious in onset, gradually progressive, upto knee region. Patient visited yasodha hospital with this complaints, used medications prescribed by them for 1 month & adviced to quit alcohol.but patient didn't quit alcohol
Not a known case of Hypertension, Diabetes, Tuberculosis, Epilepsy, Cardiovascular Accident, Coronary artery disease.
PERSONAL HISTORY:
Appetite:Normal
Diet: mixed
Sleep: Adequate
Bowel & Bladder movements: Regular
Addictions: He is a known alcoholic since 13 yrs (daily 90-180ml)
FAMILY HISTORY: Insignificant
GENERAL PHYSICAL EXAMINATION:
Patient was conscious, coherent and cooperative
moderately built and moderately nourished.
Pallor- no pallor
Icterus- no icterus
Cyanosis- no cyanosis
Clubbing- no clubbing
Generalised lymphadenopathy- no generalised lymphadenopathy
-pedal edema: B/L pitting type upto knee
And generalised edema and edema on hands.
VITALS:
On 25.09.2021
Temperature- Afebrile
Pulse rate : 72 bpm
Respiratory Rate: 18 cycles per minute
Blood Pressure: 140/90mm Hg
On 26.09.2021
Temperature- Afebrile
Pulse rate : 74 bpm
Respiratory Rate: 18 cycles per minute
Blood Pressure: 130/80 mm Hg
On 27.09.2021
Temperature: afebrile
Pulse rate: 68 bpm
Respiration: SOB during walking
Blood Pressure: 110/60 mm Hg
On 28.09.2021
Temperature: afebrile
Pulse rate: 68 bpm
Respiration: SOB
Blood Pressure: 120/60 mm Hg
On 29.09.2021
Temperature: aferbrile
Pulse rate: 78bpm
Respiration: decreased SOB
Blood Pressure: 130/80 mm Hg
On 30.09.2021
Temperature: aferbrile
Pulse rate: 84bpm
Respiration: decreased SOB
Blood Pressure: 130/80 mm Hg
Fever chart:
SYSTEMIC EXAMINATION:
CARDIOVASCULAR SYSTEM:
First and second heart sounds heard. No murmurs
RESPIRATORY SYSTEM:
Bilateral Air entry present.
CENTRAL NERVOUS SYSTEM:
Higher motor functions intact
PER ABDOMEN EXAMINATION:
Absomen - distended
Diffuse tenderness - present
INVESTIGATIONS:
RENAL FUNCTION TEST:
Blood urea: 13mg/dl
Serum Creatinine: 1mg/dl
Na+ : 141 mEq/L
K+ : 4.3 mEq/L
Cl- : 99 mEq/L
RANDOM BLOOD SUGAR : 127 mg/dl
COMPLETE BLOOD PICTURE:
Hemoglobin- 13.5g/dl
Total Leukocyte count - 9700/mm³
Neutrophils- 71%
Lymphocytes-19%
Eosinophils - 4%
Monocytes- 6%
Platelets- 3.20 lakhs/mm³
LIVER FUNCTION TEST:
Total bilirubin- 4.01 mg/dl
Direct bilirubin- 1.47 mg/dl
AST - 50 IU/L
ALT- 31 IU/L
AST:ALT - 1.6
ALP- 486 IU/L
Total protein- 5.8 g/dl
Albumin- 3.6 g/dl
Albumin:Globulin - 1.64
COMPLETE URINE EXAMINATION:
Albumin - nil
2D ECHO Report Screening:
- ' D' shape left ventricle
- Moderate TR+ EPAH: Trivial AR+/MR+
- No AS/MS
- EF= 64%
- RVSP = 38+10 = 48 mm Hg
- Good left ventricular systolic function
- No diastolic dysfunction, no PE
- Inferior venacavae size (2.24 cm) dilated
- R.A/R.V/IVC dilated
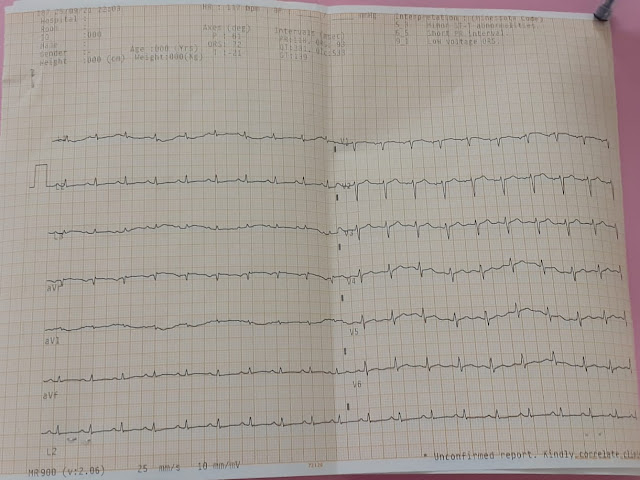
ELECTROCARDIOGRAPHY:
On 25.09.2021
DIAGNOSIS :
ANASARCA SECONDARY TO HEART FAILURE WITH WET BERI-BERI
TREATMENT:
ON 25.99.2021(day 1)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. Inj. LASIX 40 mg IV BD
3. Tab. ALDACTONE 50mg PO OD
4. ABDOMINAL GIRTH MONITORING
5. MONITORING VITALS 4TH HOURLY
6. MONITORING GRBS 12TH HOURLY
ON 26.09.2021(day 2)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. SALT RESTRICTION LES THAN 2g/day
3. Inj. LASIX 40 mg IV BD
4. Tab. ALDACTONE 50mg PO OD
5. ABDOMINAL GIRTH MONITORING
6. MONITORING VITALS 4TH HOURLY
7. MONITORING GRBS 12TH HOURLY
On 27.09.2021(day 3)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. SALT RESTRICTION LES THAN 2g/day
3. Inj. LASIX 40 mg IV BD
4. Tab. ALDACTONE 50mg PO OD
5. DAILY WEIGHT MONITORING
6. ABDOMINAL GIRTH MONITORING
7. MONITORING VITALS 4TH HOURLY
8. MONITORING GRBS 12TH HOURLY
On 28.09.2021(day 4)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. SALT RESTRICTION LES THAN 2g/day
3. Inj. LASIX 40 mg IV BD
4. Tab. ALDACTONE 100mg PO OD
5. Tab. THIAMINE 100mg PO TID
6. DAILY WEIGHT MONITORING
7. ABDOMINAL GIRTH MONITORING
8. MONITORING VITALS 4TH HOURLY
9. MONITORING GRBS 12TH HOURLY
On 29.09.2021(day 5)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. SALT RESTRICTION LES THAN 2g/day
3. Inj. LASIX 40 mg IV BD
4. Tab. ALDACTONE 100 mg PO OD
5. Tab. THIAMINE 100mg PO TID
6. DAILY WEIGHT MONITORING
7. ABDOMINAL GIRTH MONITORING
8. MONITORING VITALS 4TH HOURLY
9. MONITORING GRBS 12TH HOURLY
On 30.09.2021(day 6)
1. FLUID RESTRICTION LESS THAN 1.5LIT/DAY
2. SALT RESTRICTION LES THAN 2g/day
3. Inj. LASIX 40 mg IV BD
4. Tab. ALDACTONE 50mg PO OD
5. Tab. THIAMINE 100mg PO TID
6. DAILY WEIGHT MONITORING
7. ABDOMINAL GIRTH MONITORING
8. MONITORING VITALS 4TH HOURLY
9. MONITORING GRBS 12TH HOURLY
SOAP NOTES:
Day 1
SUBJECTIVE
- Shortness of Breathe increased on walking
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Pulse Rate - 68bpm
Blood Pressure - 140/90 mmHg
Central Nervous System - NAD
Cardiovascular System- First and second heart sounds heard
Per Abdomen - DISTENDED & TENDERNESS PRESENT
Respiratory System - Normal vesicular breath sounds heard
ASSESSMENT
- Anasarca under evaluation
- Chronic liver disease
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.TAB LASIX 40MG PO/BD
3.TAB ALDACTONE 50 MG/PO/OD
4.DAILY WEIGHT & AG MONITORING
5.BP MONITORING 8TH HRLY
Day 2:
SUBJECTIVE
- edema
- SOB increased on walking
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Pulse Rate - 74bpm
Blood Pressure - 130/80 mmHg
Central Nervous System - NAD
Cardiovascular System- First and second heart sounds heard
Per Abdomen - DISTENDED & TENDERNESS PRESENT
Respiratory System - Normal vesicular breath sounds heard
ASSESSMENT
- Anasarca under evaluation
- Chronic liver disease
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 40MG PO/BD
4.TAB ALDACTONE 50 MG/PO/OD
5.DAILY WEIGHT & AG MONITORING
6.BP MONITORING 8TH HRLY
Day 3
SUBJECTIVE
- SOB increased on walking
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Pulse Rate - 68bpm
Blood Pressure - 100/60 mmHg
Central Nervous System - NAD
Cardiovascular System- First and second heart sounds heard
Per Abdomen - DISTENDED & TENDERNESS PRESENT
Respiratory System - Normal vesicular breath sounds heard
ASSESSMENT
- Anasarca under evaluation
- Chronic liver disease
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 40MG PO/BD
4.TAB ALDACTONE 50 MG/PO/OD
5.DAILY WEIGHT & AG MONITORING
6.BP MONITORING 8TH HRLY
Day 4
SUBJECTIVE
- SOB decreased
- No fresh complaints
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Blood Pressure- 120/60 mmHg
Pulse rate - 68bpm
Central Nervous System- NAD
Cardiovascular system- S1,S2 HEARD
P/A - DISTENDED & TENDERNESS PRESENT
Respiratory System- NVBS
ASSESSMENT
- Anasarca secondary to liver disease
- CLD & Right heart failure
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 40MG PO/BD
4.TAB ALDACTONE 100 MG/PO/OD
5.TAB THIAMINE 100MG PO/TID
6.DAILY WEIGHT & AG MONITORING
7.BP MONITORING 8TH HRLY
Day 5
SUBJECTIVE
- SOB decreased
- Pain from groin to mid thigh region
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Blood Pressure- 130/80 mmHg
Pulse rate - 78bpm
Central Nervous System- NAD
Cardiovascular system- S1,S2 HEARD
P/A - DISTENDED & TENDERNESS PRESENT
Respiratory System- NVBS
ASSESSMENT
- Anasarca secondary to liver disease
- CLD & Right heart failure
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 40MG PO/BD
4.TAB ALDACTONE 100 MG/PO/OD
5.TAB THIAMINE 100MG PO/TID
6.DAILY WEIGHT & AG MONITORING
7.BP MONITORING 8TH HRLY
Day 6
SUBJECTIVE
- SOB decreased
OBJECTIVE
- patient is conscious, coherent and cooperative
Temperature: Afebrile
Blood Pressure- 130/80 mmHg
Pulse rate - 84 bpm
Central Nervous System- NAD
Cardiovascular system- S1,S2 HEARD
P/A - DISTENDED & TENDERNESS PRESENT
Respiratory System- NVBS
ASSESSMENT
- Anasarca secondary to heart failure
- wet beriberi
PLAN OF CARE
1.FLUID RESTRICTION < 1.5 LIT/DAY
2.SALT RESTRICTION < 2 GM/DAY
3.TAB LASIX 40MG PO/BD
4.TAB ALDACTONE 50 MG/PO/OD
5.TAB THIAMINE 100MG PO/TID
6.DAILY WEIGHT & AG MONITORING
7.BP MONITORING 8TH HRLY
















Comments
Post a Comment